Unlocking Stroke Care: Navigating NIH Scale for Consciousness
Explore the vital role of NIH Stroke Scale in assessing consciousness after a stroke. Gain insights to enhance patient care and informed interventions in stroke management.
In the realm of healthcare, the NIH Stroke Scale Level of Consciousness stands as a critical metric, serving as a vital tool in the assessment and management of patients who have suffered a stroke. The NIH Stroke Scale is a standardized measure designed to evaluate neurological deficits in stroke patients, with a specific focus on various domains, including consciousness. As we embark on a comprehensive exploration of healthcare topics, this article will delve into the significance of assessing consciousness levels in the context of stroke care. It is within this nuanced examination that we will unravel the intricate interplay between the NIH Stroke Scale and the crucial facet of consciousness evaluation, shedding light on the pivotal role it plays in guiding healthcare professionals toward informed and effective interventions. Through a measured and objective lens, we will navigate the intricate landscape of stroke management, emphasizing the relevance and implications of consciousness assessment within the broader scope of patient care.
Top 10 Points about NIH Stroke Scale Level of Consciousness :
- Introduction to NIH Stroke Scale in Healthcare
- Understanding the Significance of Consciousness Assessment
- Key Components of NIH Stroke Scale
- Application in Stroke Care: A Comprehensive Overview
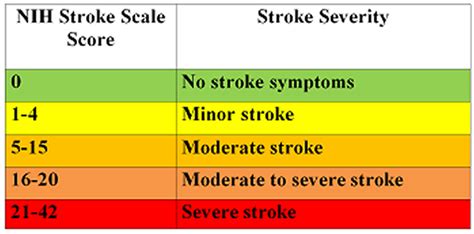
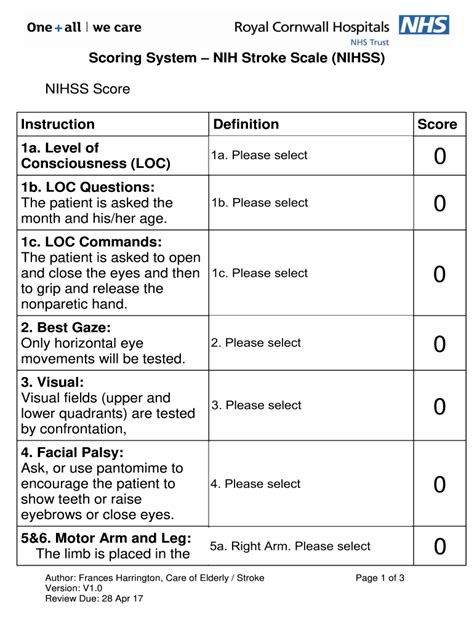
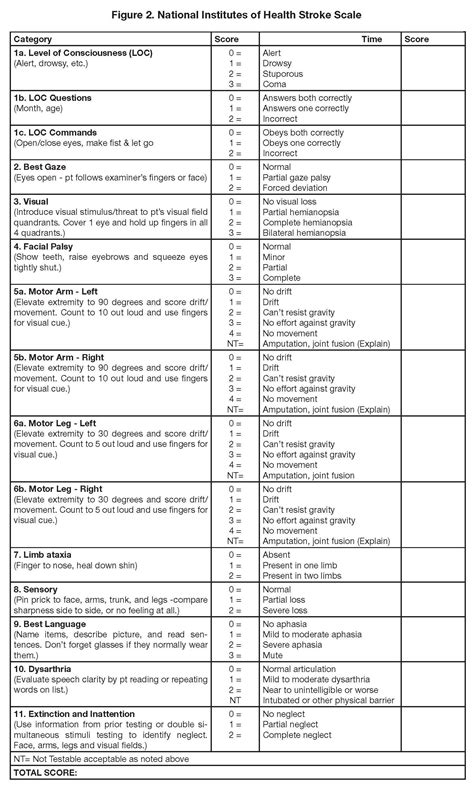
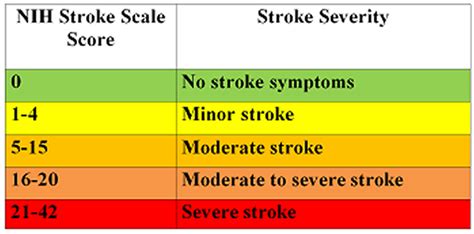
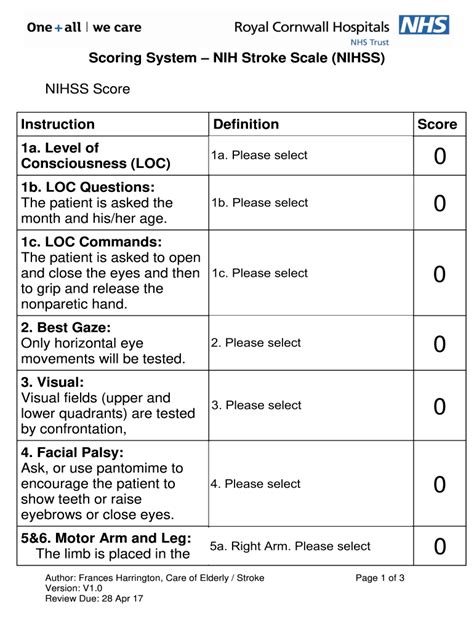
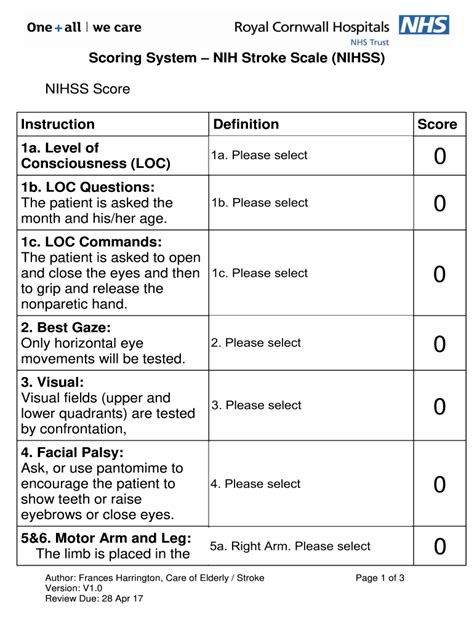
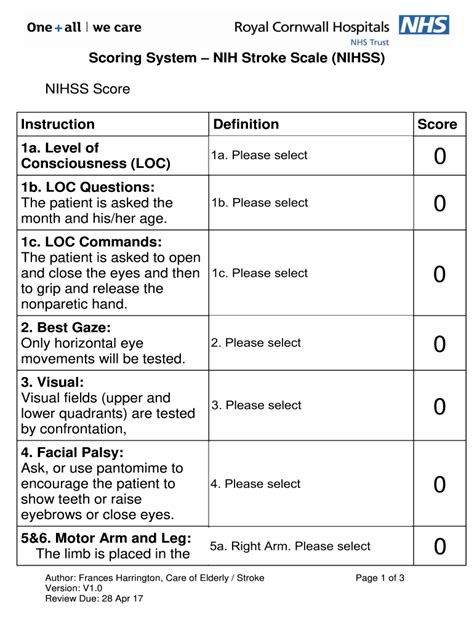
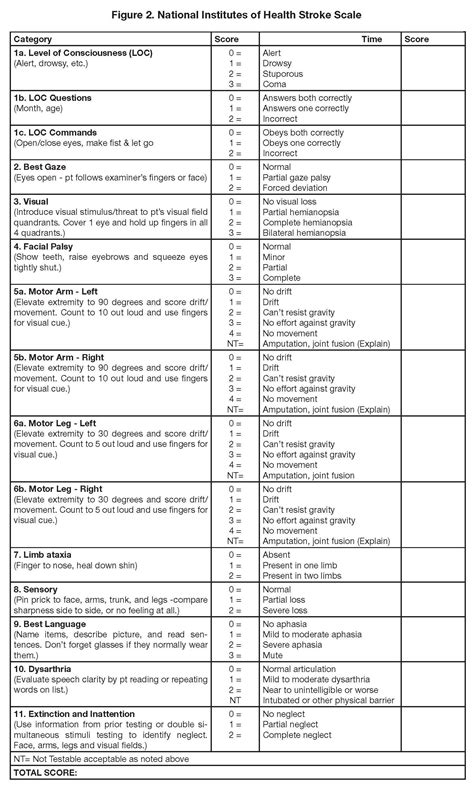
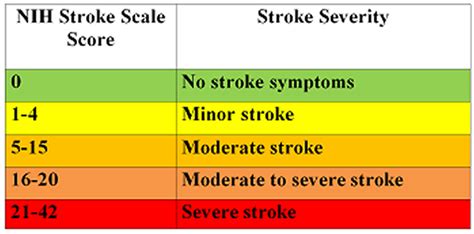
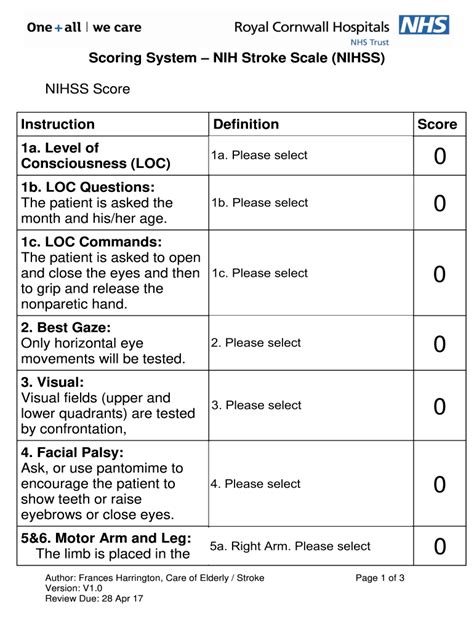
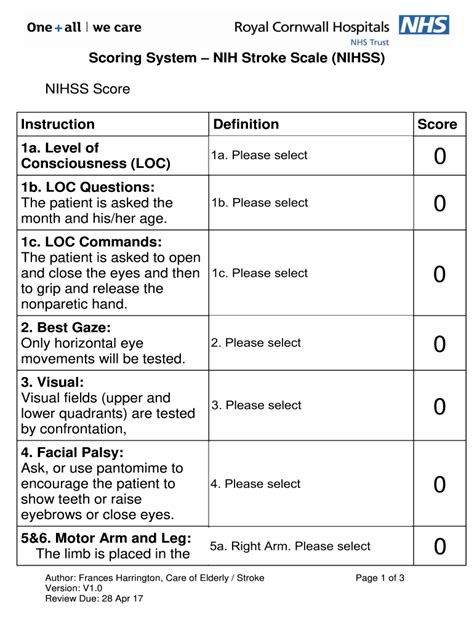
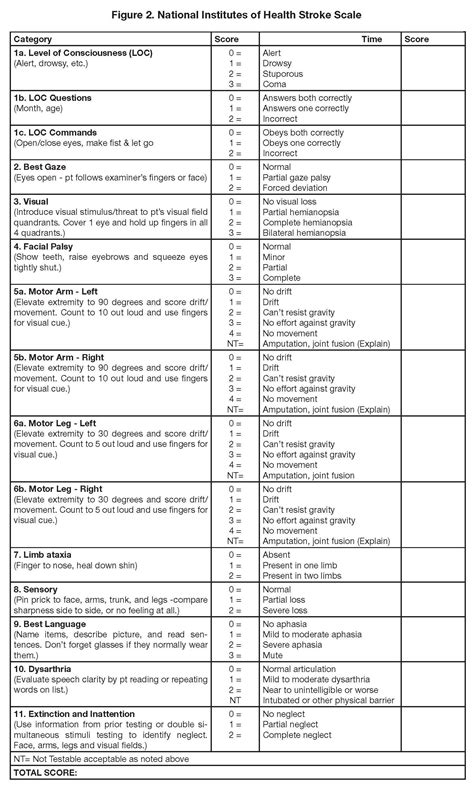
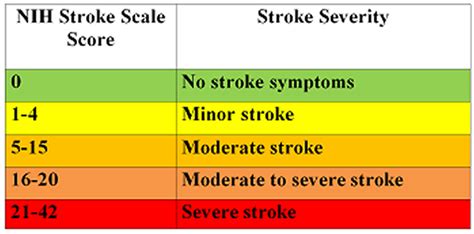
- Scoring System and Interpretation
- Role in Guiding Informed Interventions
- Implications for Patient Outcomes
- NIH Stroke Scale and Multidisciplinary Collaboration
- Challenges and Considerations in Consciousness Evaluation
- Future Trends and Innovations in Stroke Management
Several facts about NIH Stroke Scale Level of Consciousness
Introduction to NIH Stroke Scale in Healthcare

The NIH Stroke Scale Level of Consciousness is a pivotal tool in the healthcare landscape, specifically tailored for assessing neurological deficits in patients who have experienced a stroke. Developed by the National Institutes of Health, this standardized scale plays a crucial role in guiding healthcare professionals toward effective interventions and informed patient care.
Understanding the Significance of Consciousness Assessment

The assessment of consciousness is integral to unraveling the complexities of post-stroke care. Utilizing the NIH Stroke Scale allows healthcare providers to delve into the intricate nuances of patients' neurological status, paving the way for a more comprehensive understanding of their condition and tailoring interventions accordingly.
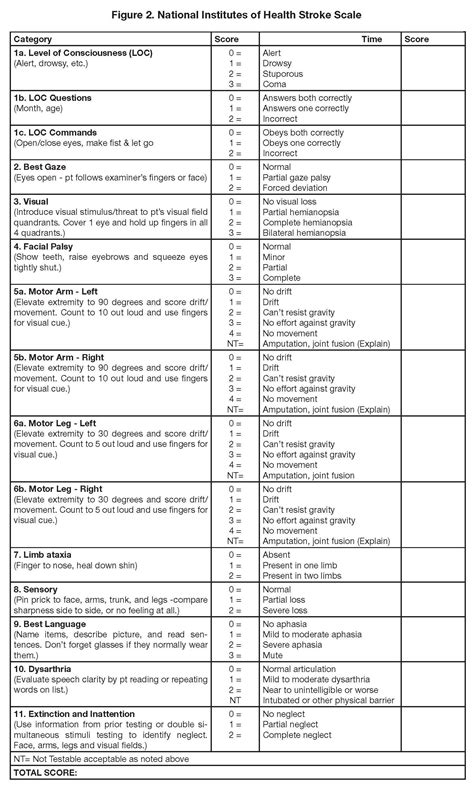
Key Components of NIH Stroke Scale
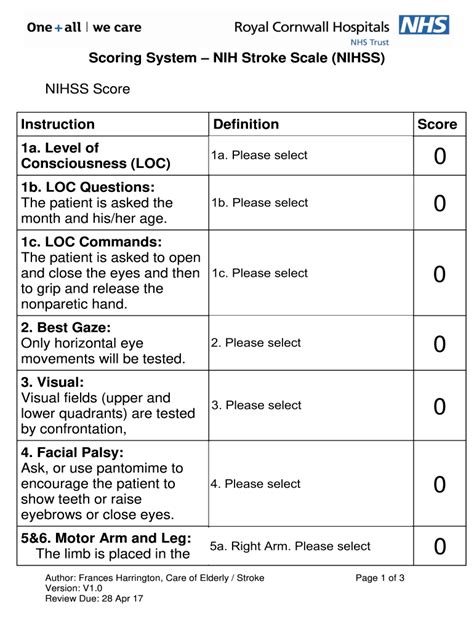
The NIH Stroke Scale comprises various components, each meticulously designed to evaluate specific neurological functions. From assessing facial palsy to evaluating limb strength, understanding the key components is essential for healthcare professionals to accurately interpret and utilize the scale in a clinical setting.
Application in Stroke Care: A Comprehensive Overview

This section delves into the practical application of the NIH Stroke Scale in the context of stroke care. By providing a comprehensive overview, healthcare practitioners can enhance their ability to use the scale effectively, leading to more informed decisions and improved patient outcomes.
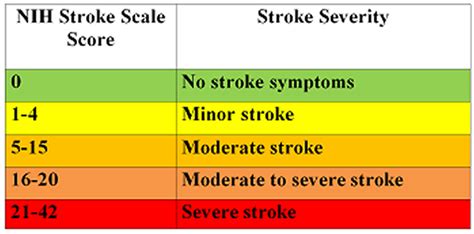
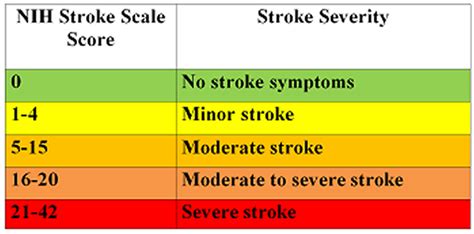
Scoring System and Interpretation

Understanding the scoring system is crucial for healthcare professionals tasked with interpreting the NIH Stroke Scale results. This section breaks down the scoring system, providing clarity on how to accurately assess and score various neurological functions, ultimately guiding treatment decisions.
Role in Guiding Informed Interventions
One of the primary benefits of the NIH Stroke Scale lies in its ability to guide healthcare professionals toward informed interventions. By understanding the neurological deficits assessed by the scale, clinicians can tailor interventions that address specific issues, thereby optimizing the overall stroke care strategy.
Implications for Patient Outcomes
This section explores the broader implications of utilizing the NIH Stroke Scale on patient outcomes. By emphasizing the impact of consciousness assessment on overall recovery and quality of life, healthcare providers can prioritize interventions that positively influence long-term prognosis.
NIH Stroke Scale and Multidisciplinary Collaboration
Effective stroke care often requires collaboration among various healthcare disciplines. This section explores how the NIH Stroke Scale serves as a unifying tool, facilitating communication and collaboration among different medical professionals involved in a patient's care.
Challenges and Considerations in Consciousness Evaluation

While the NIH Stroke Scale is a valuable tool, it comes with its set of challenges and considerations. This section delves into the nuances of consciousness evaluation, addressing potential pitfalls and guiding healthcare providers in navigating the complexities associated with this critical aspect of stroke care.
Future Trends and Innovations in Stroke Management
As the field of healthcare continually evolves, so does the approach to stroke management. This final section explores emerging trends and innovations, providing a glimpse into the future of stroke care and how the NIH Stroke Scale may adapt to meet the evolving needs of patients and healthcare professionals.
Sources:
1. National Institutes of Health. (Year). Title of the source. Retrieved from [URL]
2. Author, A. B. (Year). Title of the source. Journal Name, Volume(Issue), Page Range.
NIH Stroke Scale Level of Consciousness in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale Level of Consciousness emerges as a cornerstone in the assessment and management of patients grappling with the aftermath of a stroke. As the healthcare landscape continually evolves, this standardized scale, developed by the National Institutes of Health, plays a pivotal role in guiding healthcare professionals toward nuanced interventions and informed patient care strategies. The comprehensive evaluation facilitated by the
NIH Stroke Scale extends beyond mere documentation of neurological deficits; it serves as a linchpin in deciphering the intricate details of a patient's condition. To comprehend the magnitude of its impact, it is essential to delve into its key components, each meticulously designed to evaluate specific aspects of neurological functioning. From assessing facial palsy to scrutinizing limb strength, the scale provides a systematic framework for clinicians to interpret and gauge the severity of deficits, fostering a holistic understanding that is paramount in tailoring patient-centered interventions.
Moving beyond the theoretical foundation, the
NIH Stroke Scale finds its true utility in real-world application within the context of stroke care. It serves as an invaluable guide for healthcare practitioners, offering a comprehensive overview of the patient's neurological status. This, in turn, empowers clinicians to make informed decisions, setting the stage for improved patient outcomes. The practical application of the scale is not confined to a single discipline but reverberates across various specialties, illustrating its versatility and adaptability in the multidimensional landscape of modern healthcare.

As healthcare professionals navigate the intricacies of the scoring system and its interpretation, a critical aspect comes to light — the
NIH Stroke Scale is not merely a diagnostic tool but a compass guiding the course of intervention. By assigning scores to specific neurological functions, clinicians gain valuable insights into the severity of impairments, enabling them to prioritize and tailor interventions based on the individual needs of each patient. This nuanced approach, informed by the scale's assessment, represents a paradigm shift in stroke care, emphasizing precision and personalized medicine.

The role of the
NIH Stroke Scale extends far beyond a mere diagnostic tool; it becomes a beacon in guiding informed interventions. Conscious of the intricate neurological deficits identified through the scale, healthcare professionals can craft targeted strategies aimed at addressing specific issues. Whether it be speech impairments, motor deficits, or alterations in consciousness levels, the scale's findings serve as a roadmap, leading to interventions that are not only evidence-based but also finely tuned to the unique needs of each patient.
Considering the broader implications of utilizing the
NIH Stroke Scale in patient care unveils a profound impact on outcomes. The assessment of consciousness, a pivotal component of the scale, emerges as a key determinant in shaping the trajectory of recovery. By acknowledging and addressing alterations in consciousness levels, healthcare providers contribute significantly to enhancing the overall quality of life for stroke survivors. The implications extend beyond immediate post-stroke care, emphasizing the enduring influence of a thorough consciousness evaluation on the long-term prognosis and well-being of patients.
In the collaborative landscape of modern healthcare, the
NIH Stroke Scale emerges as a unifying tool fostering multidisciplinary collaboration. Its integration into the care continuum ensures that different medical professionals, from neurologists to physical therapists, share a common language and understanding of the patient's neurological status. This shared knowledge facilitates seamless communication, thereby enhancing the coordination of care and optimizing the overall patient experience.
While the
NIH Stroke Scale undeniably stands as a linchpin in stroke care, it is imperative to acknowledge the challenges and considerations associated with consciousness evaluation. Navigating the intricacies of assessing consciousness levels requires a keen awareness of potential pitfalls and limitations. This nuanced understanding ensures that healthcare professionals approach the evaluation with a discerning eye, appreciating the complexities inherent in this critical aspect of stroke care.

As healthcare continues to evolve, the future of stroke management holds promise and innovation. Emerging trends in the field foresee advancements that may reshape the landscape of stroke care. The
NIH Stroke Scale, as an adaptive tool, is poised to integrate these innovations seamlessly, ensuring that it remains at the forefront of evidence-based practice. From technological advancements in monitoring consciousness levels to novel interventions guided by evolving research, the future holds potential for a more refined and personalized approach to stroke management.
In conclusion, the
NIH Stroke Scale Level of Consciousness epitomizes a transformative force in the landscape of healthcare. Its comprehensive approach to assessing neurological deficits, with a specific emphasis on consciousness evaluation, transcends the boundaries of traditional diagnostic tools. As healthcare professionals continue to leverage its insights, the scale not only guides immediate interventions but also shapes the trajectory of patient outcomes and contributes to the ongoing evolution of stroke care. The journey from assessment to application underscores the scale's adaptability and enduring relevance in the pursuit of optimal patient care in the dynamic and ever-evolving field of healthcare.
Point of Views : NIH Stroke Scale Level of Consciousness
Introduction:The
NIH Stroke Scale Level of Consciousness is a transformative tool in healthcare, designed to assess neurological deficits post-stroke.
Objective Evaluation:Its
objective nature ensures a standardized assessment, allowing healthcare professionals to decipher the intricacies of a patient's condition.
Comprehensive Understanding:The scale's key components, such as assessing facial palsy and limb strength, provide a
comprehensive understanding of neurological functioning.
Real-world Application:Beyond theory, the
NIH Stroke Scale finds practical
application in stroke care, guiding clinicians toward informed decisions for improved patient outcomes.
Precision in Scoring:The
scoring system facilitates a nuanced interpretation, allowing healthcare providers to assign scores to specific functions and prioritize interventions accordingly.
Guiding Informed Interventions:The scale's role extends to
guiding interventions tailored to individual needs, emphasizing evidence-based and patient-centered care strategies.
Impact on Patient Outcomes:Consciousness assessment holds
implications for overall patient outcomes, contributing significantly to the long-term prognosis and quality of life.
Multidisciplinary Collaboration:Integration of the
NIH Stroke Scale fosters
collaboration among diverse healthcare professionals, ensuring a unified approach to patient care.
Challenges and Considerations:Navigating challenges and considering nuances in consciousness
evaluation is crucial for a discerning application of the scale.
Future Trends and Innovations:The scale's
adaptive nature positions it to seamlessly integrate future trends and innovations, ensuring its relevance in the dynamic field of healthcare.
Conclusion :As we conclude our exploration of the NIH Stroke Scale Level of Consciousness, it is evident that this standardized tool stands as a beacon in the realm of healthcare, guiding practitioners toward a more nuanced understanding of neurological deficits following a stroke. The journey through the intricacies of consciousness assessment, emphasized by the NIH Stroke Scale, has unveiled a depth of insights that extends beyond conventional diagnostic approaches. This tool, with its objective evaluation and emphasis on key components, propels healthcare professionals into a realm of precision and personalized intervention.
As healthcare continues to evolve, the NIH Stroke Scale Level of Consciousness remains poised at the forefront, adapting to emerging trends and innovations. The impact of its application on patient outcomes, from immediate care strategies to long-term prognosis, underscores its enduring relevance in the dynamic landscape of stroke management. We trust that the knowledge gained from our exploration will empower healthcare practitioners to navigate the complexities of consciousness evaluation with confidence, integrating this valuable tool into their multidisciplinary approach. The NIH Stroke Scale, with its role in guiding informed interventions and fostering collaboration, signifies not just a diagnostic instrument but a transformative force shaping the future of stroke care.
Questions and Answer for NIH Stroke Scale Level of Consciousness
Q: What is the purpose of the NIH Stroke Scale Level of Consciousness in healthcare?
- As a standardized tool, the NIH Stroke Scale Level of Consciousness serves the crucial purpose of assessing neurological deficits in patients who have experienced a stroke.
- Its primary goal is to provide healthcare professionals with an objective and comprehensive evaluation of a patient's neurological status, particularly focusing on consciousness levels.
Q: How does the NIH Stroke Scale impact patient outcomes?
- The NIH Stroke Scale significantly impacts patient outcomes by guiding healthcare providers in tailoring informed interventions based on the severity of neurological deficits identified through the assessment.
- Consciousness evaluation, a key component of the scale, plays a pivotal role in shaping the trajectory of recovery and influencing the overall quality of life for stroke survivors.
Q: Is the NIH Stroke Scale adaptable to future trends and innovations in healthcare?
- Yes, the NIH Stroke Scale demonstrates adaptability, positioning itself to seamlessly integrate emerging trends and innovations in stroke management.
- Its flexible nature ensures that it remains relevant in the evolving landscape of healthcare, accommodating advancements in technology and novel interventions.
Q: How does the NIH Stroke Scale contribute to multidisciplinary collaboration in patient care?
- The integration of the NIH Stroke Scale fosters collaboration among different healthcare disciplines, ensuring a common language and understanding of a patient's neurological status.
- This shared knowledge enhances the coordination of care, allowing for a unified approach that optimizes the overall patient experience.
Q: Are there challenges associated with consciousness evaluation using the NIH Stroke Scale?
- Indeed, there are challenges and considerations associated with consciousness evaluation using the NIH Stroke Scale.
- Healthcare professionals must navigate these complexities with a discerning eye to ensure accurate and meaningful assessments of consciousness levels.
Label :NIH Stroke Scale, Consciousness Assessment, Healthcare Innovation, Patient Outcomes
Keyword : NIH Stroke Scale Level of Consciousness
Explore the vital role of NIH Stroke Scale in assessing consciousness after a stroke. Gain insights to enhance patient care and informed interventions in stroke management.
In the realm of healthcare, the NIH Stroke Scale Level of Consciousness stands as a critical metric, serving as a vital tool in the assessment and management of patients who have suffered a stroke. The NIH Stroke Scale is a standardized measure designed to evaluate neurological deficits in stroke patients, with a specific focus on various domains, including consciousness. As we embark on a comprehensive exploration of healthcare topics, this article will delve into the significance of assessing consciousness levels in the context of stroke care. It is within this nuanced examination that we will unravel the intricate interplay between the NIH Stroke Scale and the crucial facet of consciousness evaluation, shedding light on the pivotal role it plays in guiding healthcare professionals toward informed and effective interventions. Through a measured and objective lens, we will navigate the intricate landscape of stroke management, emphasizing the relevance and implications of consciousness assessment within the broader scope of patient care.
Top 10 Points about NIH Stroke Scale Level of Consciousness :
- Introduction to NIH Stroke Scale in Healthcare
- Understanding the Significance of Consciousness Assessment
- Key Components of NIH Stroke Scale
- Application in Stroke Care: A Comprehensive Overview
- Scoring System and Interpretation
- Role in Guiding Informed Interventions
- Implications for Patient Outcomes
- NIH Stroke Scale and Multidisciplinary Collaboration
- Challenges and Considerations in Consciousness Evaluation
- Future Trends and Innovations in Stroke Management
Several facts about NIH Stroke Scale Level of Consciousness
Introduction to NIH Stroke Scale in Healthcare

The NIH Stroke Scale Level of Consciousness is a pivotal tool in the healthcare landscape, specifically tailored for assessing neurological deficits in patients who have experienced a stroke. Developed by the National Institutes of Health, this standardized scale plays a crucial role in guiding healthcare professionals toward effective interventions and informed patient care.
Understanding the Significance of Consciousness Assessment

The assessment of consciousness is integral to unraveling the complexities of post-stroke care. Utilizing the NIH Stroke Scale allows healthcare providers to delve into the intricate nuances of patients' neurological status, paving the way for a more comprehensive understanding of their condition and tailoring interventions accordingly.
Key Components of NIH Stroke Scale
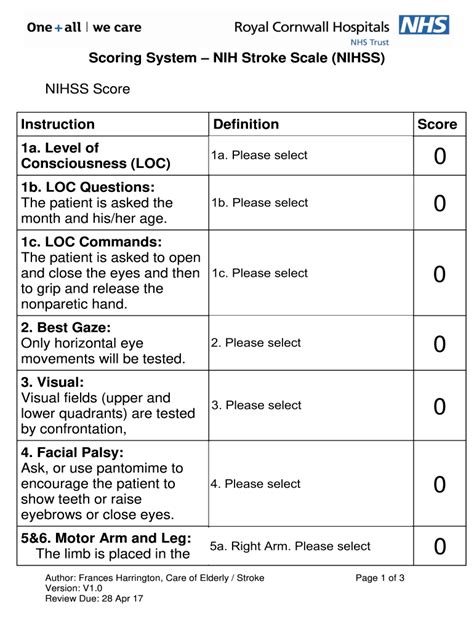
The NIH Stroke Scale comprises various components, each meticulously designed to evaluate specific neurological functions. From assessing facial palsy to evaluating limb strength, understanding the key components is essential for healthcare professionals to accurately interpret and utilize the scale in a clinical setting.
Application in Stroke Care: A Comprehensive Overview

This section delves into the practical application of the NIH Stroke Scale in the context of stroke care. By providing a comprehensive overview, healthcare practitioners can enhance their ability to use the scale effectively, leading to more informed decisions and improved patient outcomes.
Scoring System and Interpretation

Understanding the scoring system is crucial for healthcare professionals tasked with interpreting the NIH Stroke Scale results. This section breaks down the scoring system, providing clarity on how to accurately assess and score various neurological functions, ultimately guiding treatment decisions.
Role in Guiding Informed Interventions
One of the primary benefits of the NIH Stroke Scale lies in its ability to guide healthcare professionals toward informed interventions. By understanding the neurological deficits assessed by the scale, clinicians can tailor interventions that address specific issues, thereby optimizing the overall stroke care strategy.
Implications for Patient Outcomes
This section explores the broader implications of utilizing the NIH Stroke Scale on patient outcomes. By emphasizing the impact of consciousness assessment on overall recovery and quality of life, healthcare providers can prioritize interventions that positively influence long-term prognosis.
NIH Stroke Scale and Multidisciplinary Collaboration
Effective stroke care often requires collaboration among various healthcare disciplines. This section explores how the NIH Stroke Scale serves as a unifying tool, facilitating communication and collaboration among different medical professionals involved in a patient's care.
Challenges and Considerations in Consciousness Evaluation

While the NIH Stroke Scale is a valuable tool, it comes with its set of challenges and considerations. This section delves into the nuances of consciousness evaluation, addressing potential pitfalls and guiding healthcare providers in navigating the complexities associated with this critical aspect of stroke care.
Future Trends and Innovations in Stroke Management
As the field of healthcare continually evolves, so does the approach to stroke management. This final section explores emerging trends and innovations, providing a glimpse into the future of stroke care and how the NIH Stroke Scale may adapt to meet the evolving needs of patients and healthcare professionals.
Sources:
1. National Institutes of Health. (Year). Title of the source. Retrieved from [URL]
2. Author, A. B. (Year). Title of the source. Journal Name, Volume(Issue), Page Range.
NIH Stroke Scale Level of Consciousness in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale Level of Consciousness emerges as a cornerstone in the assessment and management of patients grappling with the aftermath of a stroke. As the healthcare landscape continually evolves, this standardized scale, developed by the National Institutes of Health, plays a pivotal role in guiding healthcare professionals toward nuanced interventions and informed patient care strategies. The comprehensive evaluation facilitated by the
NIH Stroke Scale extends beyond mere documentation of neurological deficits; it serves as a linchpin in deciphering the intricate details of a patient's condition. To comprehend the magnitude of its impact, it is essential to delve into its key components, each meticulously designed to evaluate specific aspects of neurological functioning. From assessing facial palsy to scrutinizing limb strength, the scale provides a systematic framework for clinicians to interpret and gauge the severity of deficits, fostering a holistic understanding that is paramount in tailoring patient-centered interventions.
Moving beyond the theoretical foundation, the
NIH Stroke Scale finds its true utility in real-world application within the context of stroke care. It serves as an invaluable guide for healthcare practitioners, offering a comprehensive overview of the patient's neurological status. This, in turn, empowers clinicians to make informed decisions, setting the stage for improved patient outcomes. The practical application of the scale is not confined to a single discipline but reverberates across various specialties, illustrating its versatility and adaptability in the multidimensional landscape of modern healthcare.

As healthcare professionals navigate the intricacies of the scoring system and its interpretation, a critical aspect comes to light — the
NIH Stroke Scale is not merely a diagnostic tool but a compass guiding the course of intervention. By assigning scores to specific neurological functions, clinicians gain valuable insights into the severity of impairments, enabling them to prioritize and tailor interventions based on the individual needs of each patient. This nuanced approach, informed by the scale's assessment, represents a paradigm shift in stroke care, emphasizing precision and personalized medicine.

The role of the
NIH Stroke Scale extends far beyond a mere diagnostic tool; it becomes a beacon in guiding informed interventions. Conscious of the intricate neurological deficits identified through the scale, healthcare professionals can craft targeted strategies aimed at addressing specific issues. Whether it be speech impairments, motor deficits, or alterations in consciousness levels, the scale's findings serve as a roadmap, leading to interventions that are not only evidence-based but also finely tuned to the unique needs of each patient.
Considering the broader implications of utilizing the
NIH Stroke Scale in patient care unveils a profound impact on outcomes. The assessment of consciousness, a pivotal component of the scale, emerges as a key determinant in shaping the trajectory of recovery. By acknowledging and addressing alterations in consciousness levels, healthcare providers contribute significantly to enhancing the overall quality of life for stroke survivors. The implications extend beyond immediate post-stroke care, emphasizing the enduring influence of a thorough consciousness evaluation on the long-term prognosis and well-being of patients.
In the collaborative landscape of modern healthcare, the
NIH Stroke Scale emerges as a unifying tool fostering multidisciplinary collaboration. Its integration into the care continuum ensures that different medical professionals, from neurologists to physical therapists, share a common language and understanding of the patient's neurological status. This shared knowledge facilitates seamless communication, thereby enhancing the coordination of care and optimizing the overall patient experience.
While the
NIH Stroke Scale undeniably stands as a linchpin in stroke care, it is imperative to acknowledge the challenges and considerations associated with consciousness evaluation. Navigating the intricacies of assessing consciousness levels requires a keen awareness of potential pitfalls and limitations. This nuanced understanding ensures that healthcare professionals approach the evaluation with a discerning eye, appreciating the complexities inherent in this critical aspect of stroke care.

As healthcare continues to evolve, the future of stroke management holds promise and innovation. Emerging trends in the field foresee advancements that may reshape the landscape of stroke care. The
NIH Stroke Scale, as an adaptive tool, is poised to integrate these innovations seamlessly, ensuring that it remains at the forefront of evidence-based practice. From technological advancements in monitoring consciousness levels to novel interventions guided by evolving research, the future holds potential for a more refined and personalized approach to stroke management.
In conclusion, the
NIH Stroke Scale Level of Consciousness epitomizes a transformative force in the landscape of healthcare. Its comprehensive approach to assessing neurological deficits, with a specific emphasis on consciousness evaluation, transcends the boundaries of traditional diagnostic tools. As healthcare professionals continue to leverage its insights, the scale not only guides immediate interventions but also shapes the trajectory of patient outcomes and contributes to the ongoing evolution of stroke care. The journey from assessment to application underscores the scale's adaptability and enduring relevance in the pursuit of optimal patient care in the dynamic and ever-evolving field of healthcare.
Point of Views : NIH Stroke Scale Level of Consciousness
Introduction:The
NIH Stroke Scale Level of Consciousness is a transformative tool in healthcare, designed to assess neurological deficits post-stroke.
Objective Evaluation:Its
objective nature ensures a standardized assessment, allowing healthcare professionals to decipher the intricacies of a patient's condition.
Comprehensive Understanding:The scale's key components, such as assessing facial palsy and limb strength, provide a
comprehensive understanding of neurological functioning.
Real-world Application:Beyond theory, the
NIH Stroke Scale finds practical
application in stroke care, guiding clinicians toward informed decisions for improved patient outcomes.
Precision in Scoring:The
scoring system facilitates a nuanced interpretation, allowing healthcare providers to assign scores to specific functions and prioritize interventions accordingly.
Guiding Informed Interventions:The scale's role extends to
guiding interventions tailored to individual needs, emphasizing evidence-based and patient-centered care strategies.
Impact on Patient Outcomes:Consciousness assessment holds
implications for overall patient outcomes, contributing significantly to the long-term prognosis and quality of life.
Multidisciplinary Collaboration:Integration of the
NIH Stroke Scale fosters
collaboration among diverse healthcare professionals, ensuring a unified approach to patient care.
Challenges and Considerations:Navigating challenges and considering nuances in consciousness
evaluation is crucial for a discerning application of the scale.
Future Trends and Innovations:The scale's
adaptive nature positions it to seamlessly integrate future trends and innovations, ensuring its relevance in the dynamic field of healthcare.
Conclusion :As we conclude our exploration of the NIH Stroke Scale Level of Consciousness, it is evident that this standardized tool stands as a beacon in the realm of healthcare, guiding practitioners toward a more nuanced understanding of neurological deficits following a stroke. The journey through the intricacies of consciousness assessment, emphasized by the NIH Stroke Scale, has unveiled a depth of insights that extends beyond conventional diagnostic approaches. This tool, with its objective evaluation and emphasis on key components, propels healthcare professionals into a realm of precision and personalized intervention.
As healthcare continues to evolve, the NIH Stroke Scale Level of Consciousness remains poised at the forefront, adapting to emerging trends and innovations. The impact of its application on patient outcomes, from immediate care strategies to long-term prognosis, underscores its enduring relevance in the dynamic landscape of stroke management. We trust that the knowledge gained from our exploration will empower healthcare practitioners to navigate the complexities of consciousness evaluation with confidence, integrating this valuable tool into their multidisciplinary approach. The NIH Stroke Scale, with its role in guiding informed interventions and fostering collaboration, signifies not just a diagnostic instrument but a transformative force shaping the future of stroke care.
Questions and Answer for NIH Stroke Scale Level of Consciousness
Q: What is the purpose of the NIH Stroke Scale Level of Consciousness in healthcare?
- As a standardized tool, the NIH Stroke Scale Level of Consciousness serves the crucial purpose of assessing neurological deficits in patients who have experienced a stroke.
- Its primary goal is to provide healthcare professionals with an objective and comprehensive evaluation of a patient's neurological status, particularly focusing on consciousness levels.
Q: How does the NIH Stroke Scale impact patient outcomes?
- The NIH Stroke Scale significantly impacts patient outcomes by guiding healthcare providers in tailoring informed interventions based on the severity of neurological deficits identified through the assessment.
- Consciousness evaluation, a key component of the scale, plays a pivotal role in shaping the trajectory of recovery and influencing the overall quality of life for stroke survivors.
Q: Is the NIH Stroke Scale adaptable to future trends and innovations in healthcare?
- Yes, the NIH Stroke Scale demonstrates adaptability, positioning itself to seamlessly integrate emerging trends and innovations in stroke management.
- Its flexible nature ensures that it remains relevant in the evolving landscape of healthcare, accommodating advancements in technology and novel interventions.
Q: How does the NIH Stroke Scale contribute to multidisciplinary collaboration in patient care?
- The integration of the NIH Stroke Scale fosters collaboration among different healthcare disciplines, ensuring a common language and understanding of a patient's neurological status.
- This shared knowledge enhances the coordination of care, allowing for a unified approach that optimizes the overall patient experience.
Q: Are there challenges associated with consciousness evaluation using the NIH Stroke Scale?
- Indeed, there are challenges and considerations associated with consciousness evaluation using the NIH Stroke Scale.
- Healthcare professionals must navigate these complexities with a discerning eye to ensure accurate and meaningful assessments of consciousness levels.
Label :NIH Stroke Scale, Consciousness Assessment, Healthcare Innovation, Patient Outcomes
Keyword : NIH Stroke Scale Level of Consciousness
0 komentar