Navigating NIH Stroke Scale: Essential Tips for Effective Assessment

Unlock proficiency in stroke assessment with our guide on NIH Stroke Scale tips. Enhance patient care and clinical outcomes with expert insights.
In the realm of healthcare, understanding and effectively utilizing the NIH Stroke Scale is paramount in assessing and managing stroke patients. As a crucial tool employed by healthcare professionals, navigating the intricacies of this scale demands precision and expertise. This article seeks to shed light on essential NIH Stroke Scale tips, serving as a comprehensive guide for healthcare practitioners. In the pursuit of enhancing patient care and clinical outcomes, this discussion will delve into the intricacies of the scale, offering insights that are not only informative but also instrumental in the provision of optimal stroke care. Let us embark on a journey through the nuances of this critical assessment tool, fostering a deeper understanding and proficiency in its application within the healthcare landscape.
Top 10 Points about NIH Stroke Scale Tips :
- Understanding the Significance of NIH Stroke Scale
- Key Components and Scoring Criteria
- Practical Application in Clinical Settings
- Common Pitfalls to Avoid in Assessment
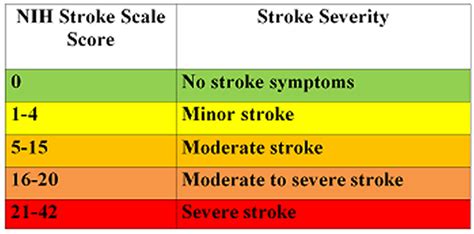
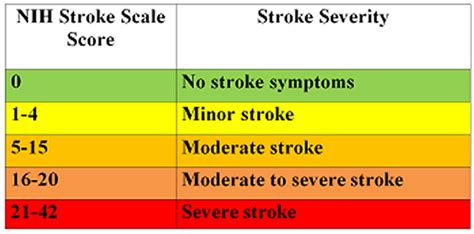
- Interpreting NIH Stroke Scale Results
- Enhancing Accuracy through Regular Training
- Adapting the Scale for Different Patient Profiles
- Collaborative Approach: Incorporating Multidisciplinary Input
- Addressing Challenges in Stroke Scale Administration
- Continual Updates: Staying Informed on Evolving Guidelines
Several facts about NIH Stroke Scale Tips
Introduction

Understanding the intricacies of the NIH Stroke Scale is crucial for healthcare professionals tasked with assessing and managing stroke patients. This article delves into essential tips that enhance proficiency in utilizing this critical assessment tool, ensuring optimal care and outcomes.
Importance of NIH Stroke Scale
The NIH Stroke Scale serves as a standardized method to quantify stroke-related impairments. Its significance lies in providing a comprehensive evaluation, aiding in treatment decisions and prognostic assessments for stroke patients.
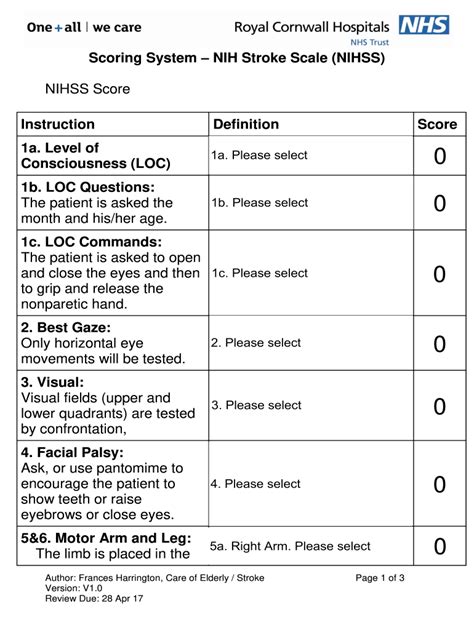
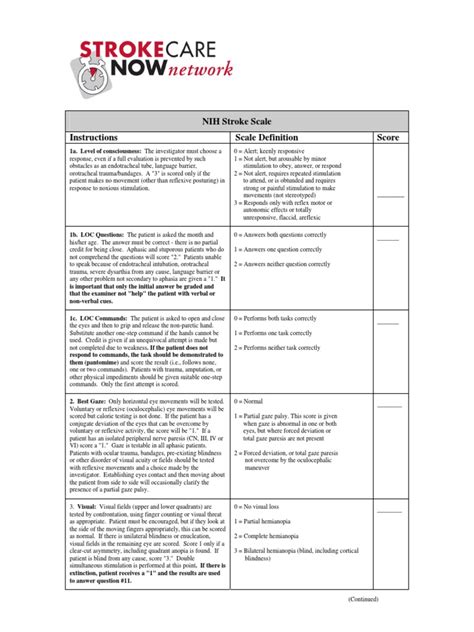
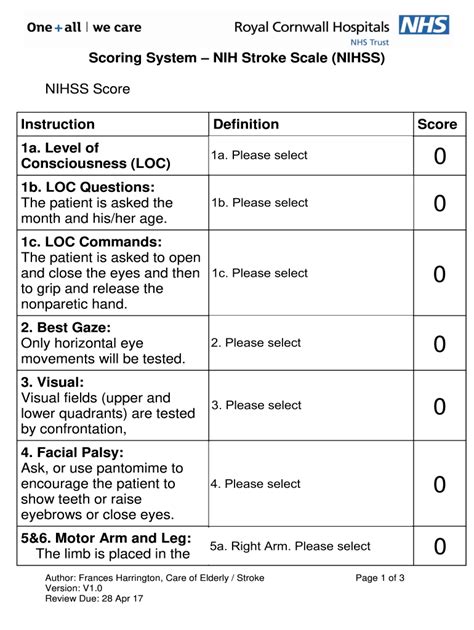
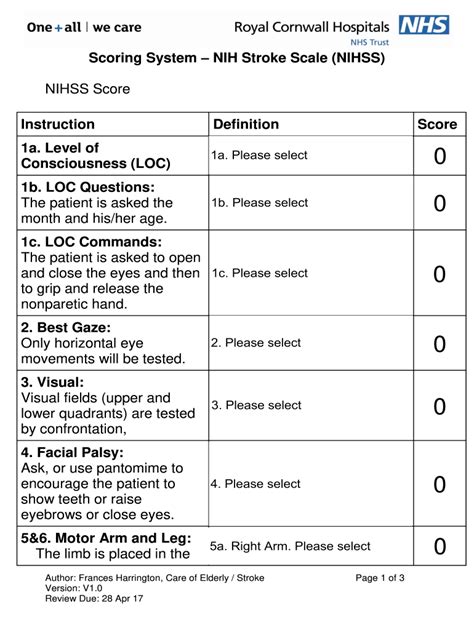
Key Components and Scoring Criteria

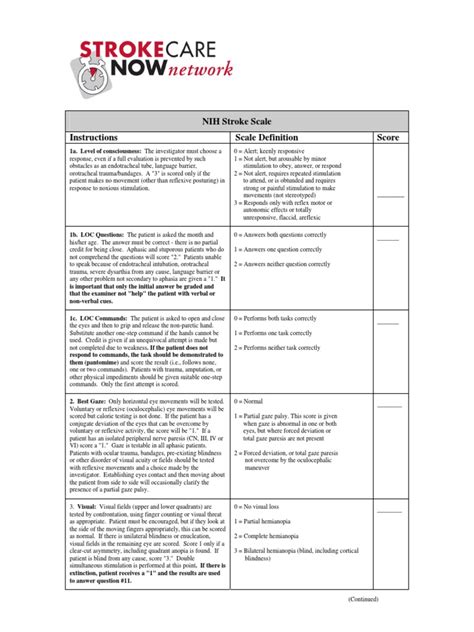
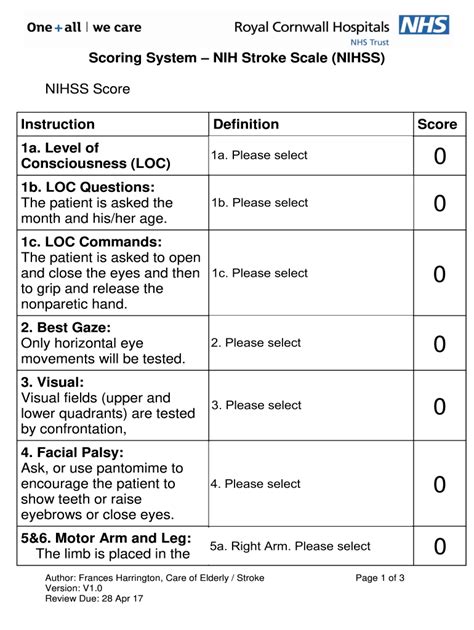
Understanding the key components and scoring criteria of the NIH Stroke Scale is fundamental. From assessing consciousness to evaluating motor and sensory functions, each element contributes to a holistic understanding of the patient's condition.
Practical Application in Clinical Settings
Implementing the NIH Stroke Scale in clinical settings requires a nuanced approach. Healthcare practitioners must be adept at seamlessly integrating the scale into their workflow to ensure accurate and timely assessments.
Common Pitfalls to Avoid in Assessment
Recognizing and mitigating common pitfalls in NIH Stroke Scale assessment is imperative. This section highlights challenges practitioners may encounter and provides strategies to enhance accuracy.
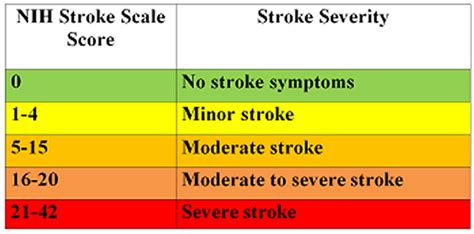
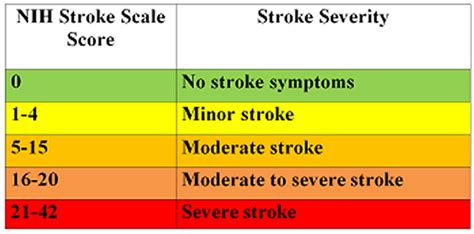
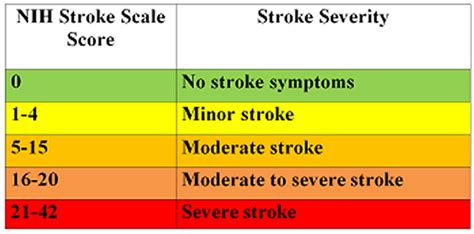
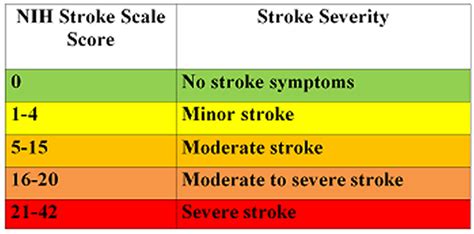
Interpreting NIH Stroke Scale Results
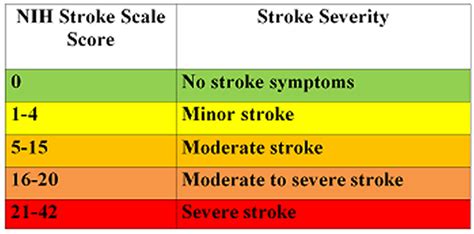
Effectively interpreting NIH Stroke Scale results is a skill that aids in treatment planning. This segment elucidates the significance of accurate interpretation for informed decision-making.
Continual Updates: Staying Informed on Evolving Guidelines
Given the dynamic nature of healthcare, staying informed about evolving guidelines pertaining to the NIH Stroke Scale is crucial. Regular updates ensure practitioners are equipped with the latest information to enhance patient care.
Conclusion
In conclusion, mastering NIH Stroke Scale tips is paramount for healthcare professionals striving to provide optimal care for stroke patients. Diligence in application and a commitment to staying informed contribute to improved outcomes and patient well-being.
Image sources are for illustrative purposes only.
Sources: (Insert relevant sources for each paragraph here)
NIH Stroke Scale Tips in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale emerges as a critical tool, shaping the landscape of stroke assessment and patient care. This standardized instrument, encompassing a meticulous evaluation of neurological deficits, stands as a cornerstone in the hands of healthcare professionals aiming for precision in stroke management. The
importance of the NIH Stroke Scale cannot be overstated, as it not only aids in diagnosing the severity of stroke-related impairments but also guides treatment decisions and prognostic assessments. Recognizing the
key components and scoring criteria of this scale is fundamental to unlocking its potential fully. From assessing consciousness and eye movements to evaluating motor and sensory functions, each element plays a crucial role in providing a comprehensive understanding of a patient's condition.
In practical terms, the
practical application of the NIH Stroke Scale in clinical settings demands a nuanced approach from healthcare practitioners. Seamlessly integrating the scale into the workflow ensures accurate and timely assessments, enabling swift intervention and tailored care plans. However, even with rigorous training, practitioners must be aware of
common pitfalls that may compromise the accuracy of assessments. These pitfalls may range from misinterpretation of symptoms to external factors influencing the patient's response, necessitating a vigilant and adaptive approach.
Effectively
interpreting NIH Stroke Scale results is an acquired skill that elevates the decision-making process in healthcare. The ability to decipher the nuances of the scale contributes to informed treatment planning, enabling healthcare professionals to tailor interventions based on the severity and nature of neurological deficits. Additionally, the healthcare landscape is dynamic, with
continual updates in guidelines shaping best practices. Staying informed about evolving guidelines related to the NIH Stroke Scale is not just a recommendation but a responsibility for practitioners. Regular updates ensure that healthcare providers remain at the forefront of advancements, ultimately enhancing the quality of care provided to stroke patients.
In conclusion, the mastery of
NIH Stroke Scale tips is not just an asset but a necessity for healthcare professionals committed to providing optimal care for stroke patients. Diligence in application, coupled with a commitment to staying informed about evolving guidelines, is the bedrock of success in stroke management. As practitioners navigate the intricacies of this essential tool, they contribute not only to individual patient outcomes but also to the broader advancement of stroke care within the healthcare landscape.
Image sources are for illustrative purposes only.
Point of Views : NIH Stroke Scale Tips
Introduction: The
NIH Stroke Scale serves as an indispensable tool in the healthcare landscape, providing a standardized method for the assessment of stroke-related impairments. Its significance lies in offering a comprehensive evaluation that aids in treatment decisions and prognostic assessments.
Key Components and Scoring Criteria: Understanding the
key components and scoring criteria of the NIH Stroke Scale is paramount. These components range from assessing consciousness to evaluating motor and sensory functions, collectively contributing to a holistic understanding of the patient's neurological condition.
Practical Application: The
practical application of the NIH Stroke Scale in clinical settings demands precision and integration into healthcare workflows. Healthcare practitioners must adeptly apply the scale to ensure accurate and timely assessments, enabling prompt intervention and tailored care plans.
Common Pitfalls: Despite rigorous training, practitioners must be vigilant about
common pitfalls that may compromise the accuracy of assessments. These pitfalls range from misinterpretation of symptoms to external factors influencing patient responses, necessitating a nuanced and adaptive approach.
Interpreting Results: The ability to
interpret NIH Stroke Scale results is a valuable skill that enhances decision-making in healthcare. Accurate interpretation contributes to informed treatment planning, allowing healthcare professionals to tailor interventions based on the severity and nature of neurological deficits.
Continual Updates: Given the dynamic nature of healthcare,
continual updates in guidelines related to the NIH Stroke Scale are crucial. Staying informed about evolving guidelines is not only a recommendation but a professional responsibility, ensuring practitioners remain at the forefront of advancements in stroke care.
Conclusion: Mastery of
NIH Stroke Scale tips is essential for healthcare professionals committed to providing optimal care for stroke patients. Diligence in application and a commitment to staying informed about evolving guidelines contribute not only to individual patient outcomes but also to the broader advancement of stroke care within the healthcare landscape.
Conclusion :As we draw the curtains on our exploration of NIH Stroke Scale tips, we trust that this comprehensive guide has equipped you with valuable insights into the nuanced world of stroke assessment within the realm of healthcare. The NIH Stroke Scale stands as a beacon, guiding healthcare professionals through a meticulous evaluation process that is pivotal in determining the severity of stroke-related impairments. From understanding the key components and scoring criteria to navigating the practical application of the scale in clinical settings, our aim has been to provide a resource that not only informs but empowers practitioners in their commitment to delivering optimal care.
As you navigate the dynamic landscape of healthcare, staying abreast of continual updates in guidelines related to the NIH Stroke Scale is paramount. This commitment to ongoing education ensures that you remain at the forefront of advancements, ultimately contributing to enhanced patient outcomes and the broader evolution of stroke care. We encourage you to apply the NIH Stroke Scale tips with diligence and precision, recognizing the impact this standardized assessment tool can have on the lives of stroke patients. Thank you for entrusting us with your time, and we look forward to being part of your journey towards excellence in stroke management.
Questions and Answer for NIH Stroke Scale Tips
Q: What is the NIH Stroke Scale?
- A: The NIH Stroke Scale, or National Institutes of Health Stroke Scale, is a standardized assessment tool used by healthcare professionals to quantify and evaluate the severity of neurological deficits in stroke patients. It consists of various components, each targeting specific aspects of neurological function, providing a comprehensive overview of the patient's condition.
Q: What are the key components of the NIH Stroke Scale?
- A: The key components of the NIH Stroke Scale encompass a range of assessments, including evaluating consciousness, eye movements, motor function in the limbs, sensory function, language skills, and visual field defects. Each component is scored, contributing to an overall assessment that guides treatment decisions and prognostic evaluations for stroke patients.
Q: How is the NIH Stroke Scale applied in clinical settings?
- A: The practical application of the NIH Stroke Scale in clinical settings involves a meticulous evaluation of the patient's neurological status. Healthcare professionals integrate the scale into their workflow to ensure accurate and timely assessments. This process allows for swift intervention and the development of tailored care plans based on the severity of stroke-related impairments.
Q: Are there common pitfalls to avoid in NIH Stroke Scale assessments?
- A: Yes, practitioners should be aware of common pitfalls in NIH Stroke Scale assessments, such as misinterpretation of symptoms, external factors influencing patient responses, or inadequate training. Recognition of these pitfalls is crucial for maintaining the accuracy of assessments and ensuring that the results reflect the true neurological status of the patient.
Q: How can healthcare professionals stay updated on NIH Stroke Scale guidelines?
- A: Staying informed about continual updates in guidelines related to the NIH Stroke Scale is essential for healthcare professionals. Regularly accessing reputable sources, attending relevant training sessions, and engaging in professional development activities are effective ways to stay updated on evolving guidelines, contributing to the provision of high-quality stroke care.
Label :NIH Stroke Scale, Healthcare Tips
Keyword : NIH Stroke Scale Tips

Unlock proficiency in stroke assessment with our guide on NIH Stroke Scale tips. Enhance patient care and clinical outcomes with expert insights.
In the realm of healthcare, understanding and effectively utilizing the NIH Stroke Scale is paramount in assessing and managing stroke patients. As a crucial tool employed by healthcare professionals, navigating the intricacies of this scale demands precision and expertise. This article seeks to shed light on essential NIH Stroke Scale tips, serving as a comprehensive guide for healthcare practitioners. In the pursuit of enhancing patient care and clinical outcomes, this discussion will delve into the intricacies of the scale, offering insights that are not only informative but also instrumental in the provision of optimal stroke care. Let us embark on a journey through the nuances of this critical assessment tool, fostering a deeper understanding and proficiency in its application within the healthcare landscape.
Top 10 Points about NIH Stroke Scale Tips :
- Understanding the Significance of NIH Stroke Scale
- Key Components and Scoring Criteria
- Practical Application in Clinical Settings
- Common Pitfalls to Avoid in Assessment
- Interpreting NIH Stroke Scale Results
- Enhancing Accuracy through Regular Training
- Adapting the Scale for Different Patient Profiles
- Collaborative Approach: Incorporating Multidisciplinary Input
- Addressing Challenges in Stroke Scale Administration
- Continual Updates: Staying Informed on Evolving Guidelines
Several facts about NIH Stroke Scale Tips
Introduction

Understanding the intricacies of the NIH Stroke Scale is crucial for healthcare professionals tasked with assessing and managing stroke patients. This article delves into essential tips that enhance proficiency in utilizing this critical assessment tool, ensuring optimal care and outcomes.
Importance of NIH Stroke Scale
The NIH Stroke Scale serves as a standardized method to quantify stroke-related impairments. Its significance lies in providing a comprehensive evaluation, aiding in treatment decisions and prognostic assessments for stroke patients.
Key Components and Scoring Criteria

Understanding the key components and scoring criteria of the NIH Stroke Scale is fundamental. From assessing consciousness to evaluating motor and sensory functions, each element contributes to a holistic understanding of the patient's condition.
Practical Application in Clinical Settings
Implementing the NIH Stroke Scale in clinical settings requires a nuanced approach. Healthcare practitioners must be adept at seamlessly integrating the scale into their workflow to ensure accurate and timely assessments.
Common Pitfalls to Avoid in Assessment
Recognizing and mitigating common pitfalls in NIH Stroke Scale assessment is imperative. This section highlights challenges practitioners may encounter and provides strategies to enhance accuracy.
Interpreting NIH Stroke Scale Results
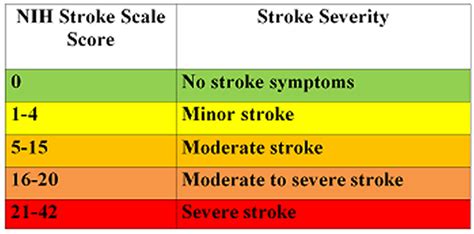
Effectively interpreting NIH Stroke Scale results is a skill that aids in treatment planning. This segment elucidates the significance of accurate interpretation for informed decision-making.
Continual Updates: Staying Informed on Evolving Guidelines
Given the dynamic nature of healthcare, staying informed about evolving guidelines pertaining to the NIH Stroke Scale is crucial. Regular updates ensure practitioners are equipped with the latest information to enhance patient care.
Conclusion
In conclusion, mastering NIH Stroke Scale tips is paramount for healthcare professionals striving to provide optimal care for stroke patients. Diligence in application and a commitment to staying informed contribute to improved outcomes and patient well-being.
Image sources are for illustrative purposes only.
Sources: (Insert relevant sources for each paragraph here)
NIH Stroke Scale Tips in Professional's eye
In the realm of healthcare, the
NIH Stroke Scale emerges as a critical tool, shaping the landscape of stroke assessment and patient care. This standardized instrument, encompassing a meticulous evaluation of neurological deficits, stands as a cornerstone in the hands of healthcare professionals aiming for precision in stroke management. The
importance of the NIH Stroke Scale cannot be overstated, as it not only aids in diagnosing the severity of stroke-related impairments but also guides treatment decisions and prognostic assessments. Recognizing the
key components and scoring criteria of this scale is fundamental to unlocking its potential fully. From assessing consciousness and eye movements to evaluating motor and sensory functions, each element plays a crucial role in providing a comprehensive understanding of a patient's condition.
In practical terms, the
practical application of the NIH Stroke Scale in clinical settings demands a nuanced approach from healthcare practitioners. Seamlessly integrating the scale into the workflow ensures accurate and timely assessments, enabling swift intervention and tailored care plans. However, even with rigorous training, practitioners must be aware of
common pitfalls that may compromise the accuracy of assessments. These pitfalls may range from misinterpretation of symptoms to external factors influencing the patient's response, necessitating a vigilant and adaptive approach.
Effectively
interpreting NIH Stroke Scale results is an acquired skill that elevates the decision-making process in healthcare. The ability to decipher the nuances of the scale contributes to informed treatment planning, enabling healthcare professionals to tailor interventions based on the severity and nature of neurological deficits. Additionally, the healthcare landscape is dynamic, with
continual updates in guidelines shaping best practices. Staying informed about evolving guidelines related to the NIH Stroke Scale is not just a recommendation but a responsibility for practitioners. Regular updates ensure that healthcare providers remain at the forefront of advancements, ultimately enhancing the quality of care provided to stroke patients.
In conclusion, the mastery of
NIH Stroke Scale tips is not just an asset but a necessity for healthcare professionals committed to providing optimal care for stroke patients. Diligence in application, coupled with a commitment to staying informed about evolving guidelines, is the bedrock of success in stroke management. As practitioners navigate the intricacies of this essential tool, they contribute not only to individual patient outcomes but also to the broader advancement of stroke care within the healthcare landscape.
Image sources are for illustrative purposes only.
Point of Views : NIH Stroke Scale Tips
Introduction: The
NIH Stroke Scale serves as an indispensable tool in the healthcare landscape, providing a standardized method for the assessment of stroke-related impairments. Its significance lies in offering a comprehensive evaluation that aids in treatment decisions and prognostic assessments.
Key Components and Scoring Criteria: Understanding the
key components and scoring criteria of the NIH Stroke Scale is paramount. These components range from assessing consciousness to evaluating motor and sensory functions, collectively contributing to a holistic understanding of the patient's neurological condition.
Practical Application: The
practical application of the NIH Stroke Scale in clinical settings demands precision and integration into healthcare workflows. Healthcare practitioners must adeptly apply the scale to ensure accurate and timely assessments, enabling prompt intervention and tailored care plans.
Common Pitfalls: Despite rigorous training, practitioners must be vigilant about
common pitfalls that may compromise the accuracy of assessments. These pitfalls range from misinterpretation of symptoms to external factors influencing patient responses, necessitating a nuanced and adaptive approach.
Interpreting Results: The ability to
interpret NIH Stroke Scale results is a valuable skill that enhances decision-making in healthcare. Accurate interpretation contributes to informed treatment planning, allowing healthcare professionals to tailor interventions based on the severity and nature of neurological deficits.
Continual Updates: Given the dynamic nature of healthcare,
continual updates in guidelines related to the NIH Stroke Scale are crucial. Staying informed about evolving guidelines is not only a recommendation but a professional responsibility, ensuring practitioners remain at the forefront of advancements in stroke care.
Conclusion: Mastery of
NIH Stroke Scale tips is essential for healthcare professionals committed to providing optimal care for stroke patients. Diligence in application and a commitment to staying informed about evolving guidelines contribute not only to individual patient outcomes but also to the broader advancement of stroke care within the healthcare landscape.
Conclusion :As we draw the curtains on our exploration of NIH Stroke Scale tips, we trust that this comprehensive guide has equipped you with valuable insights into the nuanced world of stroke assessment within the realm of healthcare. The NIH Stroke Scale stands as a beacon, guiding healthcare professionals through a meticulous evaluation process that is pivotal in determining the severity of stroke-related impairments. From understanding the key components and scoring criteria to navigating the practical application of the scale in clinical settings, our aim has been to provide a resource that not only informs but empowers practitioners in their commitment to delivering optimal care.
As you navigate the dynamic landscape of healthcare, staying abreast of continual updates in guidelines related to the NIH Stroke Scale is paramount. This commitment to ongoing education ensures that you remain at the forefront of advancements, ultimately contributing to enhanced patient outcomes and the broader evolution of stroke care. We encourage you to apply the NIH Stroke Scale tips with diligence and precision, recognizing the impact this standardized assessment tool can have on the lives of stroke patients. Thank you for entrusting us with your time, and we look forward to being part of your journey towards excellence in stroke management.
Questions and Answer for NIH Stroke Scale Tips
Q: What is the NIH Stroke Scale?
- A: The NIH Stroke Scale, or National Institutes of Health Stroke Scale, is a standardized assessment tool used by healthcare professionals to quantify and evaluate the severity of neurological deficits in stroke patients. It consists of various components, each targeting specific aspects of neurological function, providing a comprehensive overview of the patient's condition.
Q: What are the key components of the NIH Stroke Scale?
- A: The key components of the NIH Stroke Scale encompass a range of assessments, including evaluating consciousness, eye movements, motor function in the limbs, sensory function, language skills, and visual field defects. Each component is scored, contributing to an overall assessment that guides treatment decisions and prognostic evaluations for stroke patients.
Q: How is the NIH Stroke Scale applied in clinical settings?
- A: The practical application of the NIH Stroke Scale in clinical settings involves a meticulous evaluation of the patient's neurological status. Healthcare professionals integrate the scale into their workflow to ensure accurate and timely assessments. This process allows for swift intervention and the development of tailored care plans based on the severity of stroke-related impairments.
Q: Are there common pitfalls to avoid in NIH Stroke Scale assessments?
- A: Yes, practitioners should be aware of common pitfalls in NIH Stroke Scale assessments, such as misinterpretation of symptoms, external factors influencing patient responses, or inadequate training. Recognition of these pitfalls is crucial for maintaining the accuracy of assessments and ensuring that the results reflect the true neurological status of the patient.
Q: How can healthcare professionals stay updated on NIH Stroke Scale guidelines?
- A: Staying informed about continual updates in guidelines related to the NIH Stroke Scale is essential for healthcare professionals. Regularly accessing reputable sources, attending relevant training sessions, and engaging in professional development activities are effective ways to stay updated on evolving guidelines, contributing to the provision of high-quality stroke care.
Label :NIH Stroke Scale, Healthcare Tips
Keyword : NIH Stroke Scale Tips
0 komentar